
• when should intravenous hydrocortisone, ascorbic acid and thiamine be considered for treating sepsis? Table 3 occurrence of severe sepsis and deaths by clinical presentation
It’s the most common cause of death among surgical patients.
Clinical presentation of septic shock. • what interventions should be completed within first 3 hours of presentation? Clinical case scenario of septic shock. Patient may be hormo, hypo or hyper thermic i.e.
The operation resulted in 800 ml of blood loss, and she received 3000 ml of. The immune response becomes more global, more generalized to all parts of the body. Clinicians often use these terms in an imprecise manner, which adds to the confusion when describing what is meant by the term sepsis.
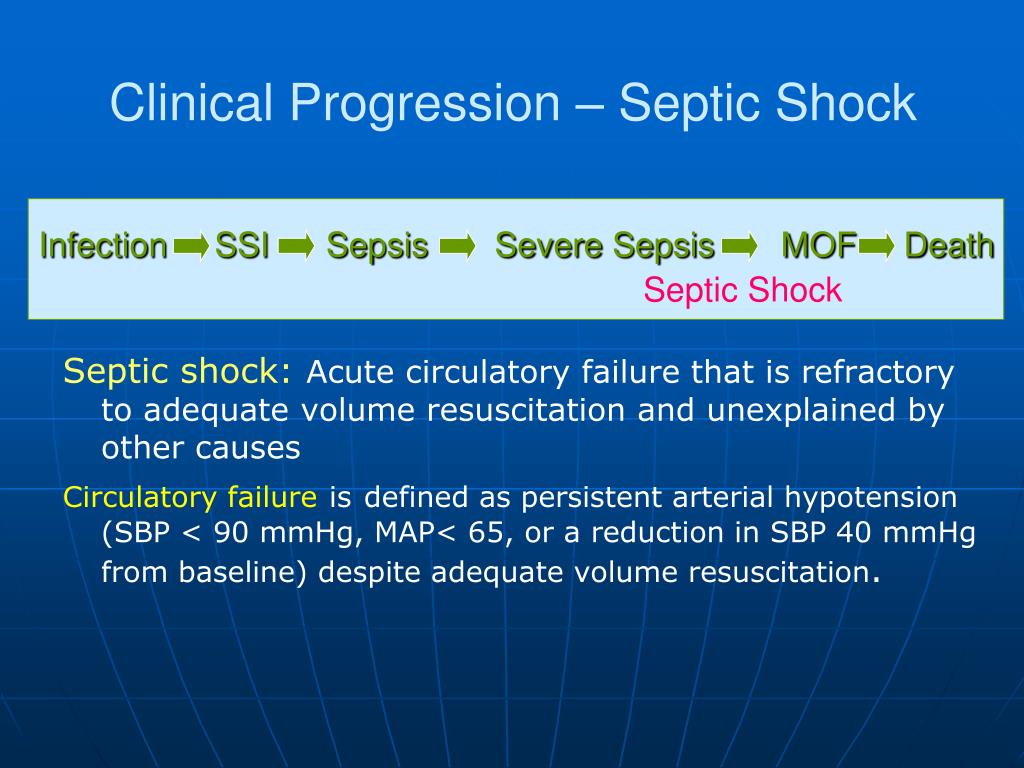
It’s the most common cause of death among surgical patients. The pathophysiology of sepsis is the result of a dysregulated host response to infection. Mild sepsis chan,ges to severe, and to septic shock.
Sepsis occurs when the inflammatory processes of the body in response to an infection exceed the boundaries of the local environment. Most patients had sepsis syndrome (69%), with 33% presenting with severe sepsis or septic shock, occurring with all clinical presentations of nts (table 3). There is some primary infection or disease.
• when should intravenous hydrocortisone, ascorbic acid and thiamine be considered for treating sepsis? A broad differential diagnosis was considered, and the focused physical examination revealing of flat neck veins and warm extremities was suspicious for a distributive shock state. Maintained on average septic shock</strong>.
The clinical presentation of sepsis is. Table 3 occurrence of severe sepsis and deaths by clinical presentation Sepsis patients exhibit a very broad spectrum of disease manifestation, ranging from relatively mild to requiring ventilation, with varied organ dysfunction, septic shock, and death.
Definition of septic shock • septic shock is a medical condition as a result of severe infection and sepsis, though the microbe may be systemic or localized to a particular site. Septic shock is described as a clinically defined subset of sepsis cases, wherein, despite adequate fluid resuscitation, patients have hypotension requiring vasopressors to maintain a mean arterial blood pressure above 65 mm hg and have an elevated serum lactate concentration of more than 2 mmol/l. Subtle changes in vital signs (eg, minimal tachycardia, widened pulse pressure, minimal tachypnea, minimally delayed capillary refill) may be the first signs of impending sirs.
Hypotension, mental status changes, and anuria are late signs. But you have to know the signs. Fever normal, low or high fever is absent in neonates, elderly, alcoholics and in uremia.
Sepsis and septic shock are clinical syndromes defined by a constellation of signs, symptoms, laboratory abnormalities and characteristic pathophysiological derangements. Perform a complete physical examination of the infant or child with suspected sepsis. With the progression of septic shock into the uncompensated stage, hypotension ensues, and patients may present with cool extremities, delayed capillary refill (more than three seconds), and thready pulses, also known as cold shock.
Clinical manifestations of septic shock usually include f ever, chills, sweating, w arm progressing to cool skin, r espiratory distress, altered mentation, decreased urine output, hypotension, elevated liver enzymes, and decreased platelet counts (mccance & huether, 2019). Sepsis (septic shock) clinical manifestations. Interactions between conserved pathogenic signals and host recognition systems initiate a systemic reaction to local infection.
As nurses at the forefront of patient care, you are uniquely positioned to make that first crucial assessment in detecting sepsis. It can cause multiple organ dysfunction syndrome (formerly known as multiple organ failure) and death. Confirmed sepsis, severe sepsis or septic shock in the emergency department or following inpatient admission.
Patients with septic shock will typically manifest signs of systemic inflammation including fever or hypothermia, tachycardia, tachypnea, and elevation or reduction of the white blood cell count. Definition shock is the clinical manifestation of failure of cellular function due to inadequate tissue perfusion and consequent cellular hypoxia resulting from a reduction in the effective circulating blood volume. Accordingly, given the clinical variability among sepsis patients there is only moderate consensus on how to accurately define the syndrome, especially at first clinical presentation.
Hypotension (sbp < 90, map < 65) or lactate > 4 mmol/l: Mortality rates from sepsis range between 25% to 30% for severe sepsis and 40% to 70% for septic shock.