As a result, gaskell et al. As a result, gaskell et al.

Management of painful neuropathy usually requires treatment with antidepressants, anticonvulsants, analgesics, and other pharmacotherapy (see table, page 20).
Diabetic neuropathic pain treatment. In addition, we will review the possibilities of pain. To help neurologists and other doctors determine the best treatment for people with diabetic neuropathy, the american academy of neurology (aan) has issued a guideline on oral and topical treatments for painful. Gabapentin and venlafaxine for the treatment of painful diabetic neuropathy.
27 rows the main classes of agents used to treat diabetic peripheral. According to the 2011 guideline issued by the american academy of neurology (aan), american academy of physical medicine and rehabilitation (aanem) and the american academy of physical medicine and rehabilitation (aapmr) guideline for the treatment of painful diabetic neuropathy (pdn), pregabalin is recommended for treatment of diabetic neuropathic. Other agents, including for topical application, such as capsaicin cream and lidocaine patches, have also been proposed to be useful as adjuvants in the control of diabetic neuropathic pain, but.
New insights and future perspectives. Although antidepressants, anticonvulsants, and opioid agonists are useful in alleviating painful neuropathy, they produce a diversity of side effects and. The guideline recommends offering one of four classes of oral medications found to be effective for neuropathic pain:
Submit your manuscript to this special issue published by journal of ophthalmology. Diabetic neuropathic pain is a common complication of diabetes and the most common form of neuropathic pain. Some less common types of peripheral neuropathy may be treated with medicines, such as:
Venlafaxine extendedrelease in the treatment of painful diabetic neuropathy: Rowbotham mc, goli v, kunz nr, lei d. Management of painful neuropathy usually requires treatment with antidepressants, anticonvulsants, analgesics, and other pharmacotherapy (see table, page 20).
Several adjuvants such as the anticonvulsive agent gabapentin have been used to treat diabetic neuropathy with several degre. This condition can be severely disabling and traditional analgesics are useless against this type of pain. Chronic neuropathic pain is generally best treated with regularly dosed medications, balancing efficacy and tolerability.
Treating neuropathic pain only 2 medications, pregabalinand duloxetine, have received regulatory approval for the treatment of neuropathic pain in diabetes by the united states federal drug agency (fda), health canada, and the european medicines agency (ema). Please refer to the full guideline at www.aan.com for more information, including definitions of the classifications of evidence and Basic concept in management of painful diabetic neuropathic is exclusion of the other cause of painful peripheral neuropathy, improving glycemic control for prophylaxis therapy and medication use for alleviating pain.
Neuropathic pain is a syndrome that affects around 1% of population. Treatment of painful diabetic neuropathy this is a summary of the american academy of neurology (aan) guideline update regarding pharmacologic and nonpharmacologic treatment of painful diabetic neuropathy (pdn). Chart with medications used to treat neuropathic pain, including diabetic peripheral neuropathy, fibromyalgia, and postherpetic neuralgia.
Found no studies of oxycodone for any other neuropathic pain conditions. Painful neuropathy in diabetic population is popular, impacting numerous chronic diabetic patients. As a result, gaskell et al.
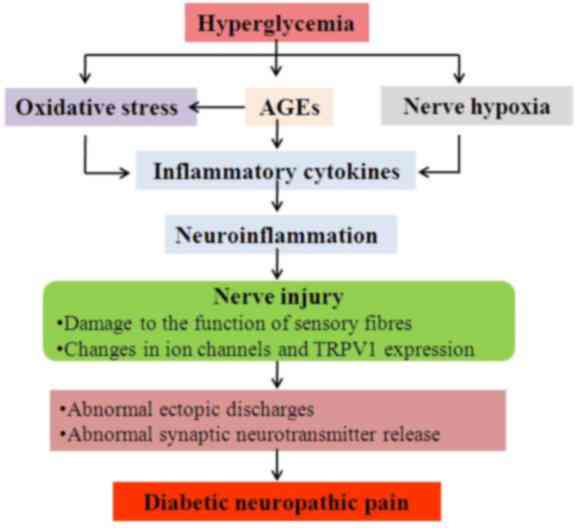
Diabetic neuropathic pain is a common complication of diabetes and the most common form of neuropathic pain. The opioid, tapentadol, has regulatory approval in the united states and canada. Nerve pain caused by diabetes, known as diabetic peripheral neuropathy, can be severe, constant, and hard to treat.it may start as a tingling feeling, followed by numbness and pain.
Furthermore, in conducting their literature search, gaskell et al.