
Bone marrow transplantation & hla typing. Your immune system uses these markers to recognize which cells belong in.
All were transplanted on prospective trials.
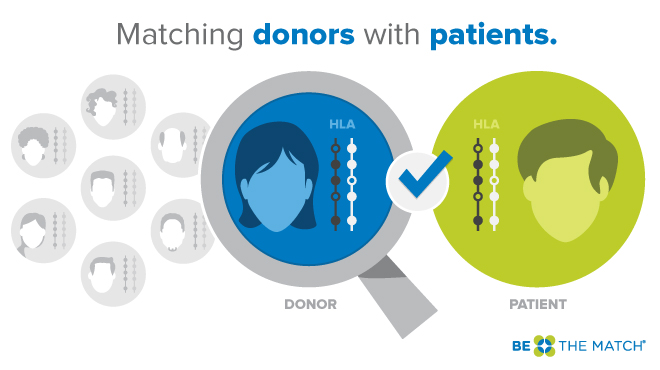
Hla matching for bone marrow transplant. In bone marrow transplants, matching is extremely important. Second, patients with graft rejection and/or graft loss had. Human leukocyte antigen (hla) typing is used to match patients and donors for bone marrow or cord blood transplants.
1 hla antigens in allografts, in allogeneic leukocytes in transfusions, and in. A new test for genetic matching in bone marrow transplantation developed by a west australian specialist is. Hla molecules are also alloantigens that can trigger immune recognition and graft rejection in unmatched recipients.
38 source of hematopoietic stem cells had been bone marrow, but mobilized peripheral blood stem cells have become more popular, and the use of umbilical. However, many patients do not have a suitable family member to serve as a donor. Human leukocyte antigen typing is not the same as abo blood typing.
Donor matching with less than 5 out of 6 hlas won’t work for a stem cell transplant using bone marrow. Bone marrow is not only the source of red blood cells that carry oxygen, but also the source of white blood cells that make up our immune system. Human leukocyte antigen (hla) typing is used to match a potential recipient with a donor for a bone marrow or cord blood transplant.
Bone marrow transplant match testing, or human leukocyte antigen (hla) typing, is a blood test used to identify the best donor for a transplant recipient. All were transplanted on prospective trials. Your immune system uses hla markers to know which cells belong in your body and.
Hla stands for human leukocyte antigen, but it is almost always referred to as hla. However, cord blood transplants don’t require exact matches, so an hla score of less than 5 out of 6 often works just as well. As a result, outcomes after transplantation have become more similar across risk categories.
Allogeneic hematopoietic stem cell transplantation is used to treat hematologic malignancy, severe aplastic anemia, severe congenital immunodeficiencies, and selected inherited metabolic diseases. First reported therapeutic use of human bone marrow cells. This is much more complex than matching blood types.
The process is critical for identifying which people can safely donate bone marrow, cord blood, or an organ to a person who needs a transplant. As a result, outcomes after transplantation have become more similar across risk categories. Ideally, a brother, sister or possibly another family member can serve as the bone marrow donor.
Bone marrow transplantation & hla typing. The best bone marrow donor is an identical twin, followed by an hla matched sibling. Biological significance of hla locus matching in unrelated donor bone marrow transplantation.
What happens when someone is looking for that perfect hla match for a patient needing a bone marrow or stem cell transplant? A blood sample is obtained so that hla proteins on the surface of white blood cells may be tested; What are my odds of matching?
Your immune system uses these markers to recognize which cells belong in. Many centers require at least a 7 of 8 loci match for bone marrow or pbsc transplants. Note that individual transplant centers may have additional matching requirements, i.e.
First doctors look at siblings because they stand the best chance of matching because they have the same mother and father and come from the same “blood pool” if you will. 2 analysis of a large cohort in the united states also indicated that hla allele mismatching is a significant risk factor for severe. The best marrow transplant outcomes happen when a patient’s human leukocyte antigen (hla) and the hla of a registry member or cord blood unit closely match.